Diabetic Foot: Causes, Signs, and Effective Treatment
Diabetes is a chronic condition that affects millions of people worldwide, and one of its most serious complications is diabetic foot. If left unmanaged, it can lead to infections, ulcers, and even amputation. Understanding the signs and knowing how to care for your feet can help prevent long-term damage.

What Is Diabetic Foot?
Diabetic foot refers to a range of foot complications caused by prolonged high blood sugar levels. These complications often result from two major factors:
-
Peripheral Neuropathy – Nerve damage that reduces sensation in the feet, making it difficult to feel injuries or pressure.
-
Peripheral Arterial Disease (PAD) – Reduced blood flow to the lower limbs, which impairs the body’s ability to heal wounds and fight infections.

4 Possible Signs of Diabetic Foot
-
Numbness, Tingling, or Burning Sensation
These symptoms are early signs of peripheral neuropathy. Patients may not feel cuts, blisters, or pressure, increasing the risk of unnoticed injuries. -
Dry and Cracked Skin
Damage to nerves can decrease sweat and oil production, resulting in dry, flaky skin. Cracks in the skin can become entry points for bacteria. -
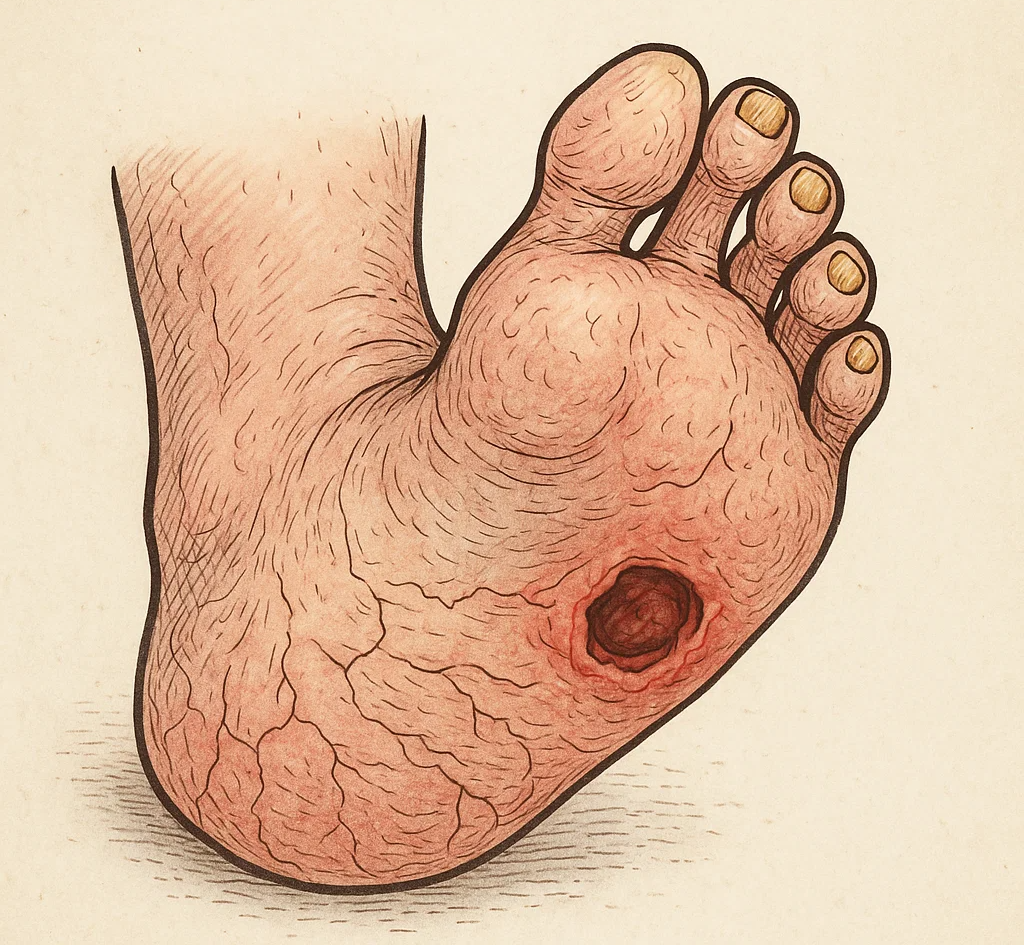
Slow-Healing Wounds or Foot Ulcers
Sores that do not heal within a few days may indicate underlying circulation problems. These ulcers can become infected and require medical attention. -
Discoloration, Swelling, or Deformity
Redness, swelling, or changes in skin color can be signs of infection or reduced blood flow. In severe cases, tissue death (gangrene) may occur, requiring urgent treatment.

Who Is at Risk?
-
People with poorly controlled blood sugar
-
Long-term diabetics (usually more than 10 years)
-
Smokers
-
Individuals with high blood pressure or high cholesterol
-
People who walk barefoot or wear ill-fitting shoes

How to Prevent Diabetic Foot Complications
1. Monitor Blood Sugar Levels
Keeping your blood glucose within the target range helps prevent nerve and vascular damage.
2. Inspect Your Feet Daily
Look for blisters, cuts, redness, swelling, or nail changes. Use a mirror to check the soles or ask for help if needed.
3. Practice Proper Foot Hygiene
-
Wash your feet daily with warm water and mild soap.
-
Dry thoroughly, especially between the toes.
-
Apply moisturizer to prevent dryness, avoiding the toe spaces.
4. Wear Proper Footwear
Choose supportive shoes with soft interiors. Avoid high heels, sandals, or going barefoot—even indoors.
5. See a Podiatrist Regularly
Routine foot exams by a healthcare professional can detect issues early and prevent complications.
Treatment Options for Diabetic Foot
If diabetic foot complications arise, treatment may include:
-
Wound Care: Cleaning, dressing, and debriding ulcers.
-
Antibiotics: To treat infections.
-
Surgical Intervention: In severe cases, such as abscesses or gangrene.
-
Blood Sugar Management: Intensive control to support healing.
In advanced cases, patients may require vascular surgery to restore blood flow or, in extreme situations, amputation to prevent the spread of infection.
Conclusion
Diabetic foot is a serious yet preventable complication of diabetes. Early recognition of symptoms and proactive foot care play a critical role in reducing the risk of ulcers and amputation. If you have diabetes, treating your feet with daily attention is not optional—it’s essential.
If you notice any unusual changes in your feet, consult a healthcare provider immediately. Timely intervention can save your feet—and your life.